This World Sight Day, we’ve compiled some of the many highlights from UNSW researchers and students working towards improving eye health.
UNSW researchers are improving access to eye care for people around the world. Image: Unsplash
To celebrate this year’s , we’re shining light on recent UNSW Sydney research in fields of optometry and vision science.
From training optometrists in Uganda to working with opthamologists in Papua New Guinea, UNSW researchers are improving access to eye care for people around the world. Closer to home, they are also finding ways to better manage glaucoma and discovering ways that eye health can indicate other illness in the body.
Read on to learn more about these exciting discoveries.
Giving the gift of sight in Papua New Guinea

Photo: Brien Holden Vision Institute
With only 10 ophthalmologists servicing a country of 7 million people, there aren’t many services available to the vision impaired in Papua New Guinea (PNG). Dr Anthea Burnett, Visiting Scholar with UNSW Optometry and Vision Science and Global Research Manager for the Brien Holden Vision Institute (BHVI), is working to change that.
Dr Burnett worked closely with local ophthalmologists, PNG Eye Care and partners to secure funding from the Fred Hollows Foundation to undertake a national survey. As part of this survey, they visited 100 communities across the country, by boat, by road, by airplane and by trekking up mountains, to interview and examine 5000 adults over the age of 50, to find out exactly how much blindness and vision impairment there was in PNG.
“PNG is a country that desperately needs this kind of research and eye care intervention. So far, my work has primarily involved finding out how widespread a problem vision impairment is, and investigating the quality of life of people with vision problems and their access, if any, to eye care services,” Dr Burnett says.
“Working in the eye care field is so rewarding because often the solutions are simple and so cheap, but have a profound impact on people’s lives.”
Find out more:
UNSW team helps revolutionise eye care for millions

Dr Kathleen Watt and Associate Professor Isabelle Jalbert with students at the Makerere University Optometry and Vision Science Teaching Clinic.
A group of UNSW Sydney academics have formed a partnership with Makerere University in Kampala, Uganda, to train optometrists and transform access to eye care services for thousands of people affected by poor vision.
The team, led by Associate Professor Isabelle Jalbert and Dr Kathleen Watt from the School of Optometry and Vision Science, are overseeing the training of local optometrists, the creation of specialist eye health programs and curriculum development for the first optometry degree ratified in Uganda.
“There are less than 10 practising optometrists in Uganda to service about 40 million people, all of who received their training overseas,” says Dr Jalbert. “It’s a really young profession and there is a huge need to train and build up the workforce to provide primary eye care.”
The team from UNSW Science, supported by UNSW’s Institute for Global Development, are spending the next year visiting Makerere University to teach students and support the faculty, particularly in specialised fields of advanced contact lenses training, binocular vision, paediatric optometry, and ocular diseases.
Find out more:
Collaboration between eye care professionals improves glaucoma management
Optometrists and ophthalmologists at UNSW’s Centre for Eye Health are taking a new approach to managing patients with glaucoma.
The Glaucoma Management Clinic, a collaboration between the Prince of Wales Hospital Ophthalmology Department and the UNSW Centre for Eye Health, was developed to relieve some of the pressure on public hospitals. This clinic is the first of its kind in Australia.
Optometrists refer patients with suspected glaucoma to the clinic where specially trained optometrists carry out advanced testing and recommend a management program in collaboration with ophthalmologists.
“This new model of care we have established has great potential to help with the challenge to assess new, non-urgent outpatient referrals for glaucoma to public hospital ophthalmology within the 4-month regulatory requirement,” says study co-author and ophthalmologist Dr Michael P. Hennessy.
Find out more:
Non-invasive detection of cancer in the eye
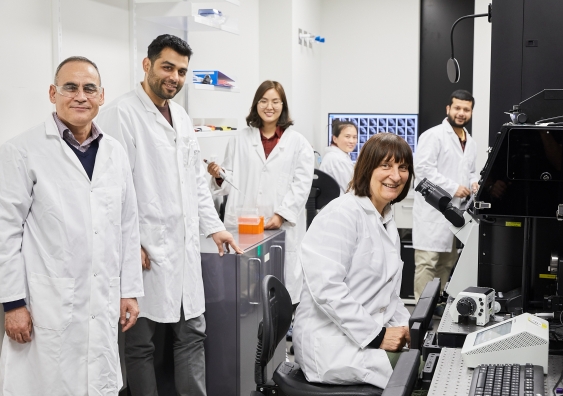
Professor Ewa Goldys and her team use the power of biophotonics: using the colours and shapes of cells and tissues to diagnose and treat disease.
Professor Ewa Goldys, Deputy Director of the Australian Research Council (ARC) Centre of Excellence for Nanoscale BioPhotonics (CNBP), has announced the development of a new, automated, non-invasive technique for diagnosing eye surface cancer (ocular surface squamous neoplasia).
The innovative method comprises the custom-building of an advanced imaging microscope in association with state-of-the-art computing and artificial intelligence operation. The results will make it possible to identify between diseased and non-diseased eye tissue, in real-time, through a simple imaging process using automated systems.
“We have been able to detect the presence of cancer on the surface of the eye, in addition to mapping the location of abnormal tissue margins,” says Goldys.
“This is a breakthrough because the only alternative way of diagnosing ocular cancer is through a biopsy. We can replace this unpleasant procedure by taking a colour photograph, which is completely unique in ophthalmology at present.”
Find out more:
Tear samples could help detect diabetes complication

Tear sample collection in process. Photo: UNSW
Tear-testing may be the future of screening for diabetic peripheral neuropathy, a debilitating condition that affects people with diabetes, new research from UNSW Sydney suggests.
The study, recently published in , is the first to show that peripheral nerve damage – often the earliest sign of the condition – can be traced in tear film.
“We found that people with type 1 diabetic peripheral neuropathy – which can result in recurring ulcers of the feet and in severe cases require amputation – have reduced levels of a protein known as ‘substance P’ in their tear film,” says Dr Maria Markoulli, senior author of the study.
“119,000 Australians have type 1 diabetes. In the future, they may be able to have a quick tear sample collected either at their optometrist, the chemist, GP or endocrinologist, and be told whether they are at risk.”
Find out more: