Adrian Krainer and Richard Finkel receive the K. J. Zülch Prize for their development and testing of a drug for spinal muscular atrophy
Although spinal muscular atrophy is a rare condition, it is the most common gene-related cause of death in children. This year, The Gertrud-Reemtsma Foundation is awarding the K. J. Zülch prize to a scientist and a clinician who have been developing and testing a new drug to combat this condition: Adrian Krainer at the Cold Spring Harbor Laboratory led a research team that developed antisense agents to combat spinal muscular atrophy, and tested them in mice. These tests met with such success that they led to testing of the drug Nusinersen in clinical trials led by Richard Finkel, a physician at Nemours Children’s Hospital. This was the first time a drug improved patients’ motor skills and significantly extended their survival. Nusinersen was approved at the end of 2016, and more than 7,500 patients have benefitted from its effects. The K. J. Zülch Prize, with a value of 50,000 euros, will be awarded on 12 September, 2019 in Cologne.
In Germany, about 300 children are born every year with spinal muscular atrophy, a degenerative disorder of a type of nerve cells. Up until just a few years ago, the diagnosis was a death sentence for many newborns.
About half of the patients develop the severe type I form of the condition. These children develop the first symptoms of muscle weakness either in the uterus or during their first months of life. They never learn to sit or crawl and usually die of respiratory failure and related infections before their second birthday. Children with the intermediate type II form usually live longer and can sit independently, but are confined to a wheelchair for life and have a shortened life expectancy. In the milder type III and type IV forms, the onset of the condition does not occur until later in childhood or adulthood and allows those affected to live a broadly normal life, albeit with a decline or loss of ambulation.
All patients with spinal muscular atrophy have one genetic defect in common: they lack SMN1, the gene responsible for production of the SMN (survival of motor neurons) protein. This protein is required to prevent the progressive death of a specific type of nerve cells in the spinal cord and brain stem, cells which are responsible for transmitting signals from the brain to the body’s muscles. However, humans have an almost identical second version of the gene: the SMN2 gene. Unfortunately, a largely defective transcript is made from this gene, and only a small amount of functional protein is produced as a result. The more copies of the SMN2 gene a patient has, the more functional SMN protein can be produced by that backup gene, and the milder the effects of the condition. Various research approaches are therefore focused on increasing the protein production from the SMN2 gene.
Erroneous splicing
As a biochemist, Adrian Krainer has been researching for decades how genes are transcribed and translated into proteins, and how the underlying mechanisms can be influenced. During gene transcription into RNA, sequences containing information for the protein, called exons, must be separated from non-coding sections (introns) and joined together. This editing process is known as RNA splicing. However, a mutation in an exon of the SMN2 gene causes that exon to be omitted most of the time during RNA splicing, producing only a truncated protein, which rapidly degrades.
Adrian Krainer has been researching a type of molecule that can be used to correct the defective RNA splicing. The so-called antisense oligonucleotides, are short RNA-like segments which bind to specific sites on the transcript of a gene and influence how the information from the gene is converted into protein. In the case of defective SMN2 RNA splicing, Krainer found a short segment of 18 nucleotides that would aid production of the entire protein.
In collaboration with Ionis Pharmaceuticals, Krainer used mice that do not produce their own SMN protein, but instead have two copies of the human SMN2 gene, to test their antisense oligonucleotides, called Nusinersen. These mice develop severe spinal muscular atrophy and die within ten days of birth. However, when Krainer’s team administered Nusinersen before the onset of symptoms, the mice developed no muscle atrophy, and survived for over 250 days.
Clincal studies with Nusinersen
Following these promising results, Richard Finkel and colleagues investigated the effectiveness and potential side effects of Nusinersen in clinical trials. These trials also produced astonishing results. In a study of infants with the type I disorder, the original intention was to determine whether the survival of non-ventilated patients was extended by administering Nusinersen. However, it soon became clear that patients were also developing well and achieving motor milestones, as a result of Nusinersen treatment.
The results of an interim analysis of the study were so positive that it became ethically unreasonable to withhold Nusinersen from the placebo group. These infants were then enrolled into another study, in order for them to also benefit from the drug. Finkel realized that for the first time a drug significantly alleviates or reverses the reduction in patients’ movement and extends survival. As a result of the successful clinical trials, Nusinersen was approved as a drug in the US at the end of 2016, with approximately 7,500 patients worldwide being treated with it to date.
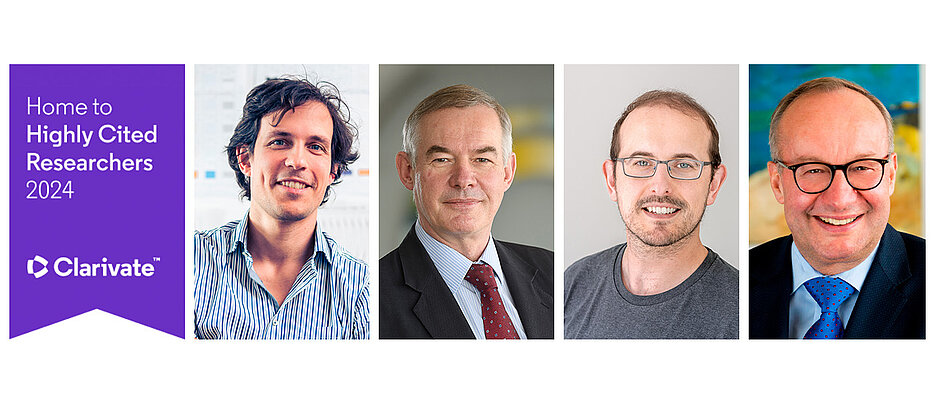
The Prize Winners
Adrian Krainer studied biochemistry at Columbia University and earned his doctorate in biochemistry and molecular biology from Harvard University. To continue his research career, he moved to Cold Spring Harbor Laboratory, where he first carried out postdoctoral research, and then obtained a professorship. He has been a full professor there since 1994 and St. Giles Foundation Professor since 2009.
After studying chemistry and medicine, Richard Finkel moved to Harvard Medical School where he specialized in paediatrics and neurology. He subsequently worked as a paediatrician and neurologist in hospitals in Denver and Philadelphia. He is currently Professor of Neurology at the University of Central Florida and Head of Neurology at Nemours Children’s Hospital in Orlando.
The K. J. Zülch Prize
The K. J. Zülch Prize 2019 will be presented at 4:30 pm on 12 September, 2019 at Cologne’s Historic City Hall. Following laudation from Brunhilde Wirth from the University of Cologne, Adrian Krainer will present a report on new precision medicines for neurological disease. After a laudation from Stephan Zierz from the University Halle-Wittenberg, Richard Finkel will give a speech on rescuing spinal muscular atrophy by antisense oligonucleotide therapy.