With the exponential rise of COVID-19 globally, a key problem is the burden outbreaks place on hospitals. Beds, ventilators and ICU wards are at capacity – overwhelmed and unable to cope with the sheer speed of transmission.
and the team at the University’s are fast-tracking the development of a biomarker that aims to determine how a patient with a positive COVID-19 test may respond to the virus. The biomarker is revealed by a blood test that requires drops of a patient’s blood to see how their immune system is responding.
“When our body is being attacked by the virus, the immune system gets switched on. When it gets switched on, it starts telling all the other immune cells to come and fight the virus. During that process, the immune system gives out a lot of dangerous signals and that is what we’re measuring through this blood test,” said Associate Professor Tang.
The aim of the test is to assist doctors to interpret these signals and assess whether or not the patient is at risk.
For example, it would provide doctors with vital information on patients who have immune systems that may fail in the next 24 hours. On the converse, it would be able to identify patients who have immune systems able to fight the virus. This would assist doctors to triage and prioritise most at-risk patients.
Current tests available only test for the virus, they do not give insight into how the body may respond.
“This test, among other things, will help doctors to make informed decisions.”
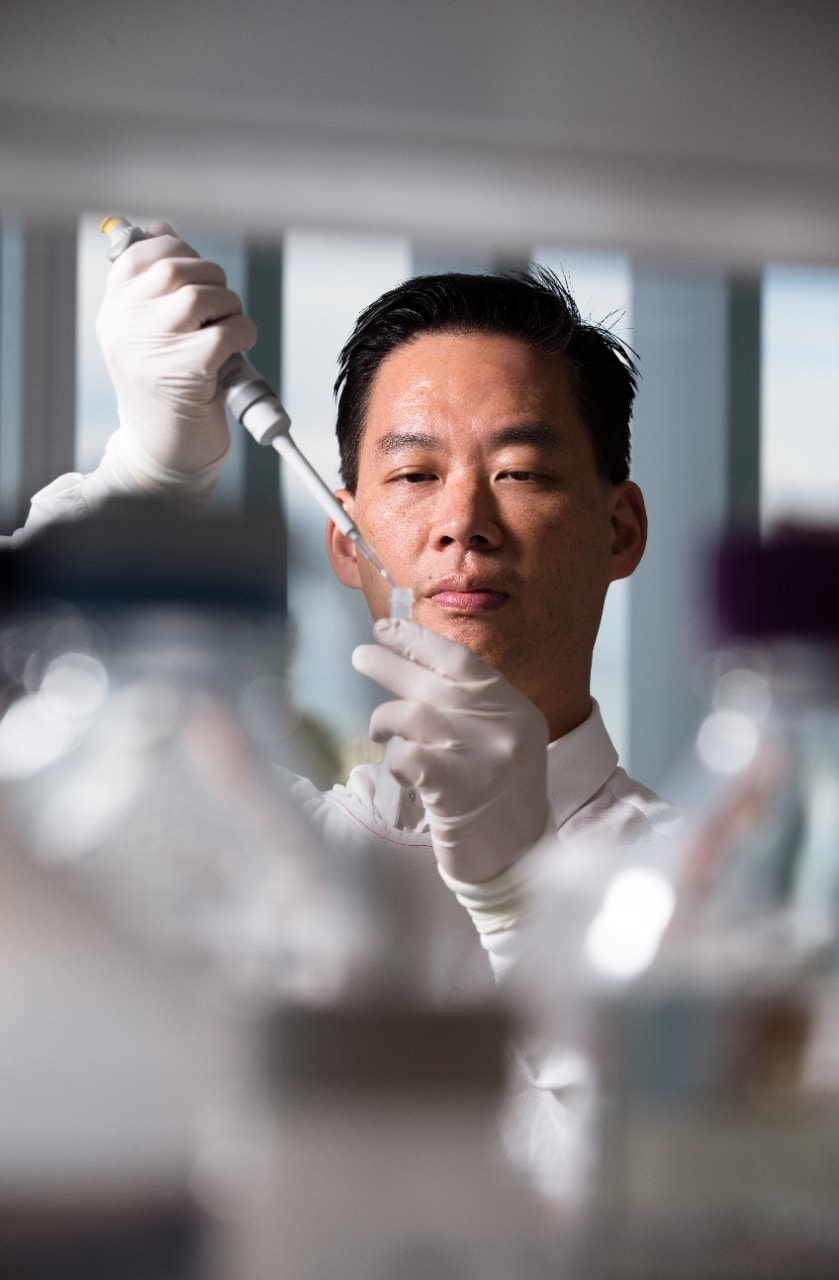
Associate Professor Benjamin Tang Photo: Janie Barrett / The Sydney Morning Herald
“It’s not enough just to know that they are infected, we need to know which patient you can send home and which patient you should admit to hospital, or which patient you need to refer to ICU,” said Associate Professor Tang.
“It’s also important from a public health point of view on a national level because there will be limited resources when the COVID-19 crisis accelerates.
“This test, among other things, will help doctors to make informed decisions.”
Researchers predict that the sooner the test is proven effective, and doctors have access to it, the more equipped our hospitals will be to fight COVID-19.
The , launched this week, will support fast-tracking this research into practice.
Under normal circumstances, the development and testing process would take more than five years.
Associate Professor Tang and his team are hoping to complete this work in five weeks with the following action plan:
- Phase 1 aims to reach 500 samples. “We need to test more samples just to be confident in our results. We’re confident that it will because we’ve been doing coronavirus research for 10 years,” Associate Professor Tang says.
- Phase 2 aims to increase the turnaround of test results by hiring and training more staff. Currently, Associate Professor Tang has a small team who are able to turnaround samples within 24 hours. “The turnaround time for individual samples is only a few hours, but to actually process [a larger number of] samples, you need people running it through 24/7. So, that will be the major bottleneck,” says Associate Professor Tang.
- Phase 3 aims to translate this into a diagnostic service and have enough manpower to run the test and provide a report to hospitals across Australia.
“We’re really racing against time. The virus is moving fast, much faster than we can manage. Every minute that goes past, someone else in the world is dying. We really need to get this out as soon as possible,” said Associate Professor Tang.
Declaration: Associate Professor Tang declares no competing interests. This project is currently in phase 1, continuing work will be subject to ethics approval and peer-review processes.
Hero image: Associate Professor Benjamin Tang at work in the lab Photo credit: Janie Barrett / The Sydney Morning Herald








