With up to 40 percent of COVID-19 deaths attributed to heart failure, the work shows immense promise and the researchers are eager to see it progress to human studies.
The study, published in , details a method of implanting the assistive pump into the main heart chamber guided by three-dimensional wide-angle intracardiac ultrasound – used for the first time in Australia as part of the study.
It was made possible by the state-of-the-art facilities at the University of Sydney’s , part of a Core Research Facility based at the and Royal Prince Alfred Hospital.
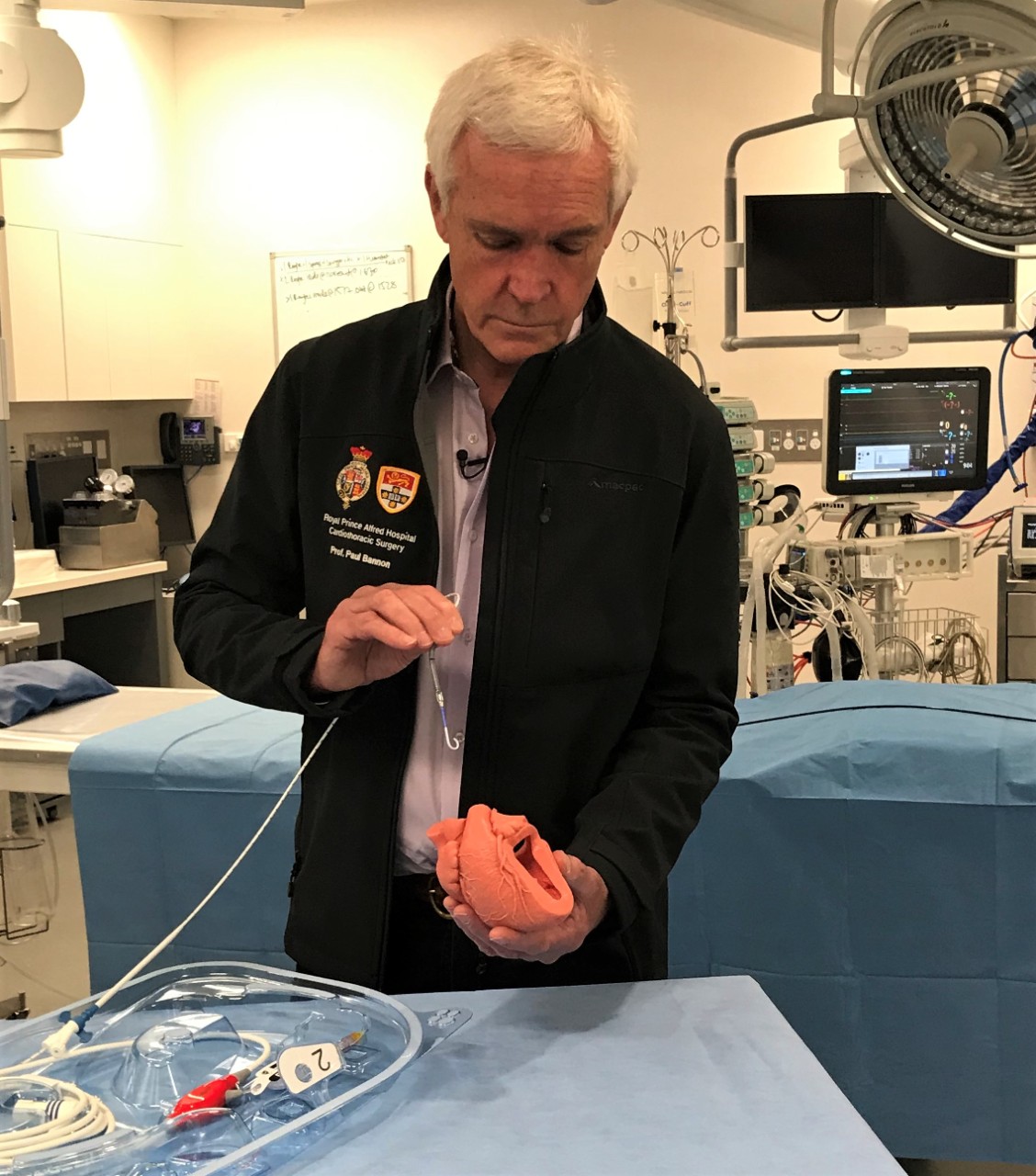
Professor Bannon demonstrates the placement of the pump
“This study provides a strong basis for researchers to progress to human studies implanting the mechanical pump inside the left ventricle of the heart using three-dimensional intracardiac ultrasonography as a guide, and without ever having to transport the patient,” said lead author , Professor and Chair of Cardiothoracic Surgery in the Faculty of Medicine and Health, Deputy Director of the Hybrid Theatre, Sydney Imaging and Head of Cardiac Surgery at Royal Prince Alfred Hospital.
“As well as all critically ill and unstable patients, this has potential to benefit the sickest COVID-19 patients who may not be able to be moved to the catheterisation laboratory or operating theatre for the traditional procedure due to isolation requirements.”
Unlike traditional ultrasound where probes go onto the skin, three-dimensional intracardiac ultrasound goes inside the blood vessels and is navigated inside the heart.
“The 3D ultrasound images are taken from inside the heart and this results in much better-quality images that can assist in complex procedures such as this,” said Professor Bannon.
The mechanical pump used in the study is a left ventricular assist device currently in use in Australia. It is used for patients undergoing high-risk heart interventions through the skin or in instances where the heart is failing to pump enough blood to support the body.
The translational study was conducted with sheep to replicate heart anatomy similar to humans.
Inside Sydney Imaging’s Hybrid Theatre
The Hybrid Theatre, a Core Research Facility based at the Charles Perkins Centre, combines a range of biomedical imaging technologies, artificial intelligence, robotics and pioneering surgical practice and training. Image-guided and robotic surgery are used to develop and perfect the complex surgical procedures of tomorrow, resulting in less invasive techniques and better outcomes.
Professor Bannon says the term ‘hybrid’ represented a new way of performing surgeries – a hybrid of traditional open surgeries in addition to the less invasive procedures the theatre supports.
“The Hybrid Theatre also represents a hybrid between the massive technological and academic strengths of the University of Sydney, and the drive for innovative and effective treatments from the hospitals we partner with,” he added.
Declaration: This work was supported by The Baird Institute (for applied heart and lung surgical research) and Royal Prince Alfred Hospital. The Impella CP® pumps and Impella Automated Controller were provided by Abiomed. AcuNav Volume ICE catheters were provided by Siemens. Neither Abiomed or Siemens had any role in study design, data acquisition or the content of the manuscript. The authors declare no competing interests. Ethics approval was obtained (2019/1650 amendment) and guidelines and legislation governing animal studies were strictly adhered to.
Header Image: First author Associate Professor Konstantin Yastrebov explaining the use of the three-dimensional wide-angle intracardiac ultrasound.








