When Jarina Bibi first felt discomfort in her abdomen she thought she might be suffering from indigestion.
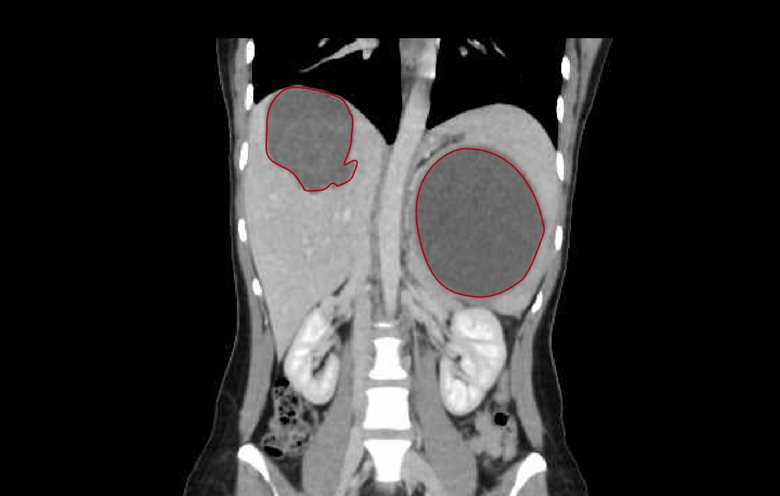
The 29-year-old had no idea that in fact she had a watermelon-sized parasitic cyst growing on her liver – a toxic timebomb that could potentially have killed her.
But thanks to the expertise of Mater doctors and their collaboration with a panel of international specialists, Bibi’s cyst was safely removed in a five-hour operation at Mater Private Hospital Brisbane.
Two secondary cysts, the size of a rockmelon and tennis ball, were also removed.
Although her spleen and parts of her liver and pancreas were removed during the procedure, Jarina is recovering well and thankful her “nightmare” illness is finally over.
Jarina moved to Brisbane from her native India to study in 2015, unaware that she had already contracted hydatid disease (also known as hydatidosis or echinococcosis).
The disease is most prevalent in Central Asia and South America. It occurs when tapeworm larvae lodge in the body and form large cysts containing eggs and a fluid that is potentially deadly to humans if the cyst is ruptured.
Humans are infected through ingestion of parasite eggs in contaminated food, water or soil, or after direct contact with animal hosts.
When Jarina’s symptoms began to include vomiting and constipation she was referred to Mater Private Hospital Brisbane gastroenterologist and hepatologist Dr Kate Cayzer, who confirmed hydatid disease after an ultrasound scan.
Jarina was referred to Mater Director of Infectious Diseases Dr Paul Griffin, who quickly concluded that surgery was necessary to treat her “extreme case”.
“The infection is not often seen in Australia, but it is something infectious diseases doctors have to be aware of,” Dr Griffin said.
“It’s a challenging disease to treat. There are a range of different treatment options, including medicines and surgery. Given the severity of her case, Jarina met the criteria for surgery.”
Fortunately, Jarina’s procedure would be in the best possible hands.
Mater general surgeon Dr Mehan Siriwardhane has a clinical interest in hepato pancreato biliary (HPB) surgery, which includes the organs of the liver, pancreas and gallbladder.
He also co-founded HPBridge – an evolving forum through which a core of 16 HPB specialists in Australia, the US, Europe and the developing world support each other’s work and study challenging cases.
In Jarina’s case, the expertise of doctors based in Myanmar provide to be invaluable.
“Jarina is quite small and, given the size of this cyst, if she had received a significant blow to her stomach there’s a real possibility it would have burst,” Dr Siriwardhane said.
“If the cyst ruptures, the fluid inside contains a protein that is poisonous to humans and it can cause the person to go into anaphylactic shock and die.
“Given the complexity of Jarina’s infection, I took her case to the forum and doctors from Myanmar – who are more familiar with this disease – were able to identify how best to treat her.
“We eventually ended up using a combination of techniques, medical and surgical, based on some of the input we got from those doctors.
“During the five-hour surgery we removed part of Jarina’s liver, her whole spleen and part of her pancreas to make sure we removed all of the disease.”
Jarina, of Calamvale, said despite the severity of her infection, she always felt confident in the care she received.
“Dr Siriwardhane made sure we figured out a plan where the disease wouldn’t come back, and in my case, it had to be traditional, rather than keyhole surgery, because of the size of the cyst,” she said.
“I do cry sometimes at the thought of something that size being inside of me for such a long time, it was like a nightmare, it still haunts me.
“It was so difficult and stressful, but I’m feeling so much better now.
“I want other people to be aware of this disease – and to know that help is available to them should they ever be affected.”
Pictured: Jarina Bibi and Mater general surgeon Dr Mehan Siriwardhane.
Pictured below: Ms Bibi’s CT scan – cysts circled in red.