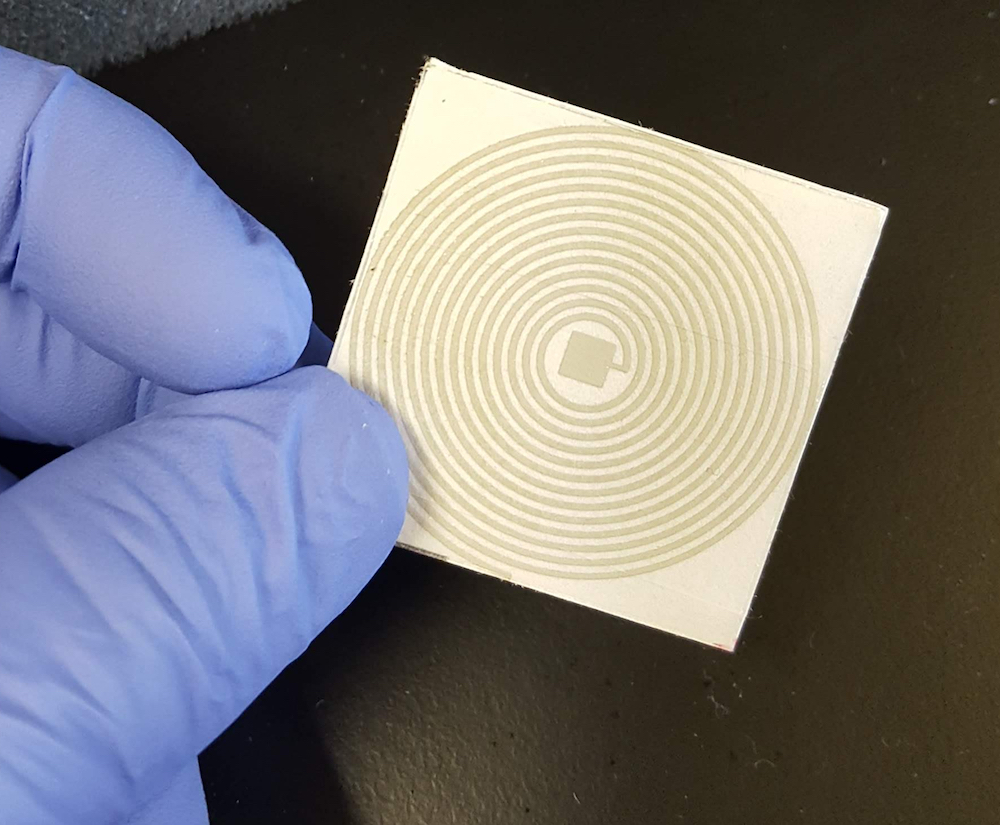
This is an example of a paper, printed sensor under development by Nigel Reuel and his research group. Larger photo. Photo courtesy of Nigel Reuel.
AMES, Iowa – There would be no tents set up in parking lots. No long lines of cars. No medical staff in full protective gear. No waiting for results.
Instead, you’d take your own COVID-19 diagnostic test at home with a $1 (or so) kit. You’d take your own nasal and cough samples. You’d spread the samples on a card. You’d stuff the card in an envelope with a virus-killing coating and let everything incubate overnight. Then you’d drop the envelope at a collection center or in the mail.
The unopened envelope would be scanned by an electronic reader to determine a positive or negative result. Then, that never-opened envelope, samples and all, would be dropped in an incinerator.
The electronic reader would automatically text or email your results.
“We’re trying to make it so that no one has to touch the samples,” said Nigel Reuel, an assistant professor of at Iowa State University. “Let’s see if we can make this possible.”
Toehold switches and reporter proteins
When he thinks about a better way to do diagnostic testing, Reuel envisions a low-cost, mail-safe, fast-scan “diagnostic platform that is well-suited for widespread monitoring of infection during pandemics,” according to a summary of his project.
Adam Carr
Reuel has a one-year, of $200,000 from the to develop the testing platform. The agency’s RAPID grants allow it to “quickly process and support research that addresses an urgent need,” according to an agency announcement.
Reuel said his idea would address several urgent testing problems: “This approach off-loads the burden of diagnostics from health workers, eliminates the increased use of limited personal protective equipment, and provides a better response to outbreaks,” he wrote.
Not only that, it would provide a real-time outbreak map with demographic details to help public health officials monitor the infection.
Key to the technology is a new sensor system based on “toehold switches” that detect target RNA genetic material. That detection triggers production of “reporter” proteins that can change the color of a sensor or, in this case, the frequency of a sensor’s signal.
During an academic conference last winter, Reuel heard more about the toehold technology from
Keith Pardee, an assistant professor with the Leslie Dan Faculty of Pharmacy at the University of Toronto, who works in partnership with Alexander Green, an assistant professor with the Biodesign Center for Molecular Design and Biomimetics at Arizona State University. They had done prior work with the Zika virus and recently demonstrated a direct, electrical interface of their toehold circuit. They’re now collaborators on Reuel’s project.
Reuel thought the toehold technology could fit some of his ideas for a closed, contact-free diagnostic sensing system using paper-based resonant sensors.
From skunkworks to telltale signals
Reuel started a side, “skunkworks” project in January and February exploring the idea of using the toehold technology as a way to find general disease targets, which quickly narrowed to targeting the coronavirus that causes COVID-19. Two doctoral students in chemical and biological dove into the details – Adam Carr on the wireless sensor and Jared Dopp on the synthetic biology.
Jared Dopp
It now looks like the finished product would involve a multilayered assembly on thick paper. The top layer would hold collected nasal or cough samples, middle layers would contain the toehold switch and bottom layers a printed, coiled resonant circuit that can be scanned for telltale frequencies.
If there’s target COVID-19 RNA in the samples, the toehold switch would allow production of proteins that degrade a coating on the circuit resulting in a positive signal. If there’s no virus RNA, there’s no protein production, no coating degradation and a negative signal.
Reuel said the technology can be tuned to detect other diseases or even future pandemics.
“The driving motivation of this project,” Reuel wrote, “is to provide a faster response to enable widespread screening and tracking of an expanding viral outbreak.”






