CAR T-cell therapy, a certain kind of cancer treatment in which the immune system’s T cells are programmed to attack tumour cells, is effective in mice with ovarian cancer, according to a study published in The Journal for ImmunoTherapy of Cancer. The researchers, who work at Karolinska Institutet, hope that the discovery will pave the way for a clinical trial to see how effective the treatment is for women with the disease.
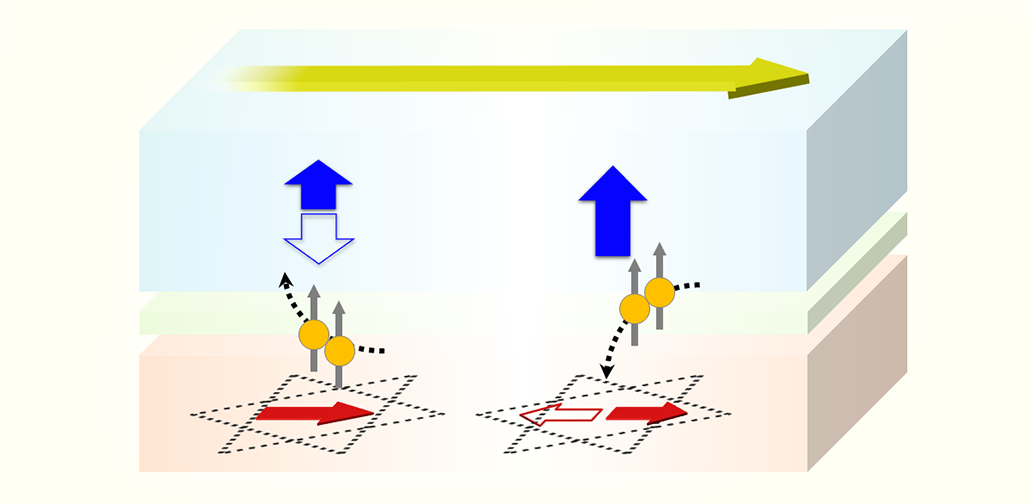
CAR T-cell therapy is a relatively new type of immunotherapy that involves extracting a patient’s immune cells (known as T cells) from the blood and injecting them in a laboratory with a new gene that specifically attacks a molecule called a chimeric antigen receptor (CAR) on the surface of the tumour cells. When returned to the patients, the T cells are more aggressive, and attack the cancer cells like guided missiles.

Isabelle Magalhaes, docent på KI.
Photo: Helen Kaipe
“This therapy is currently available for patients with blood cancer, and we want to investigate if we can use the method to treat ovarian cancer,” says the study’s joint last author Isabelle Magalhaes, docent at the Department of Oncology-Pathology at Karolinska Institutet. “Despite many improvements to the available therapy, the prognosis for women with ovarian cancer is still poor.”
Tumour environment unfavourable for T cells
Until now, CAR T-cell therapy has proved largely ineffective against solid tumours.
“Tumours often arise in an environment that’s unfavourable for T cells, in part due to a low oxygen level,” says Jonas Mattsson, visiting professor at Karolinska Institutet, and the second join last author. “This can cause attacking T cells to be neutralised, which impairs the therapeutic effect. So we wanted to examine if it would still work.”

Jonas Mattsson, gästprofessor på KI.
Foto: Bildmakarna
Many ovarian tumours contain mesothelin, and the researchers wanted to test three types of CAR molecule programmed to attack this particular protein. They therefore repeatedly exposed ovarian cancer cells to the programmed CAR T-cells in test tubes and conducted several experiments on mice.
Mice lived longer
All three CAR T-cells significantly prolonged the lives of the mice with cancer compared to those in the control group, with the type called M1xx CAR T cells proving the most efficacious. The mice that were injected with T cells that express that particular molecule saw a reduction in tumour size and lived even longer than the others. Several of the mice were even cured.
“In several mice, there were no tumor cells left that we could detect, and the effect lasted just over three months after the treatment started. This is evidence that immunotherapy involving CAR T cells that attack the mesothelin protein is a promising one for ovarian cancer,” says Professor Mattsson.
What’s the next stage of your research?
“Hopefully, this discovery will pave the way for a clinical study,” he says. “Our goal is to predict the optimal conditions for producing CAR T cells able to infiltrate and attack the tumour and survive in the bodies of women with ovarian cancer.”
The study was financed by the Swedish Cancer Society, the Swedish Childhood Cancer Foundation, the Cancer Research Funds of Radiumhemmet, the Swedish Research Council and through a donation by Jeanette and Harald Mix.
Publication: “Tuned activation of MSLN-CAR T cells induces superior anti-tumor responses in ovarian cancer models”, Esther Schoutrop, Thomas Poiret, Ibrahim El Serafi, Ying Zhao, Rui He, Alina Moter, Johan Henriksson, Moustapha Hassan, Isabelle Magalhaes, Jonas Mattsson, Journal for ImmunoTherapy of Cancer, online 6 February 2023, doi: 10.1136/jitc-2022-005691
Publikation
, Esther Schoutrop, Thomas Poiret, Ibrahim El Serafi, Ying Zhao, Rui He, Alina Moter, Johan Henriksson, Moustapha Hassan, Isabelle Magalhaes, Jonas Mattsson, The Journal for ImmunoTherapy of Cancer, online 6 februari 2023, doi: 10.1136/jitc-2022-005691