The study by The George Institute researchers, though by no means exhaustive, is indicative of alarming trends
India has a high burden of sepsis with more than one in two patients admitted to intensive care units (ICUs) across the country developing this complication with associated high rates of anti-microbial resistance and death rates, reveals a new study conducted by The George Institute for Global Health.
The study titled, “Estimates of Sepsis Prevalence and Outcomes in Adult Patients in the ICU in India: A Cross-sectional Study” was conducted in 35 ICUs across the country and was led by a multi-country team of researchers from India and Australia.
The Indian team comprised Prof. Vivekanand Jha, Executive Director and Dr. Bharath Kumar Tirupakuzhi Vijayaraghavan, Honorary Senior Fellow from The George Institute for Global Health, India. Dr Bharath is also an intensive care specialist at the Apollo Main Hospital, Chennai. The Australian team comprised A/Prof. Naomi Hammond, Lead, Critical Care Program, Dr Ashwani Kumar, PhD student, Research Associate and Prof. Bala Venkatesh, Professorial Fellow from the Critical Care Program, The George Institute for Global Health, Sydney.
“Sepsis is a global health problem. Limited data exist on the prevalence of sepsis using current definitions in ICUs in India,” says Prof Vivekanand Jha, Executive Director, The George Institute for Global Health, India, adding that the study was the first of its kind attempting to map the prevalence of sepsis in India using new consensus definitions in adult patients admitted to ICUs. “Though the study is by no means exhaustive, it is definitely indicative of alarming trends and indicates the need for further research on a larger scale.”
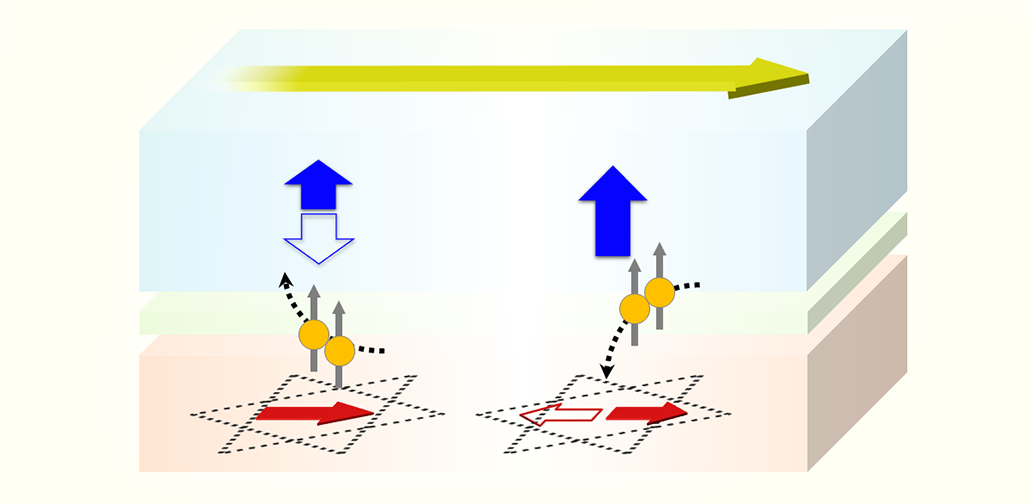
The researchers who have come together to set up the Sepsis Investigator network used consensus definitions to map the burden of sepsis and septic shock. The researchers enrolled 680 patients in 35 ICUs across the country on four separate days in 2019 to determine sepsis prevalence using the current definition and comparing it with the previous definition.
Additional outcomes included reporting on current microbiological characteristics, antimicrobial use, multidrug-resistant infections, and 30-day discharge and death rate in patients with sepsis.
“Our data highlights both the huge burden of sepsis and of antimicrobial resistance (AMR)- in many ways a ‘double whammy’. Urgent action is needed from stakeholders in order to strengthen timely recognition, improve awareness, and bolster sepsis and AMR research in India”, says Dr. Bharath Kumar, who led the Apollo team that participated in the study, adding that 382 of 677 patients (56.4%) had sepsis on the study day which is higher than the previous estimates in Indian ICUs.
“The cause of sepsis was predominately bacterial infections in 79% of patients with fungal infections causing 14% of infections. Importantly, approximately 45% of infections were caused by multidrug-resistant organisms” says A/Prof Naomi Hammond, lead author on the paper. She also added that the death rate at 30 days after the study day and rates of discharge against medical advice were significantly higher in the sepsis cohort compared to those who didn’t have sepsis.
“These findings have implications for public health and future research,” says Prof Bala Venkatesh of The George Institute, critical care program, adding that sepsis is a global health problem and the high burden of sepsis in the study cohort is cause for concern and warrants future research.
This study was funded by the Under-served Populations in LMIC Seed Grant from The George Institute for Global Health.
The paper’s online first version is published in the journal CHEST, read full paper