In first-time mothers requiring vacuum-assisted delivery, a lateral episiotomy (angled cut) in the tissue between the vaginal and anal opening more than halves the risk of obstetric anal sphincter injury, a severe form of perineal trauma between the vulva and anus. This according to a randomised clinical study led by researchers at Karolinska Institutet and Stockholm’s Danderyd Hospital, the results of which are published in The BMJ.

Obstetric Anal Sphincter Injury (OASI), which involves the anal sphincter muscles, can lead to anal incontinence with difficulties retaining gas and faeces. It can also cause sexual problems and impair quality of life. This serious form of perineal injury affects around five per cent of all first-time mothers in Sweden who have a vaginal birth.
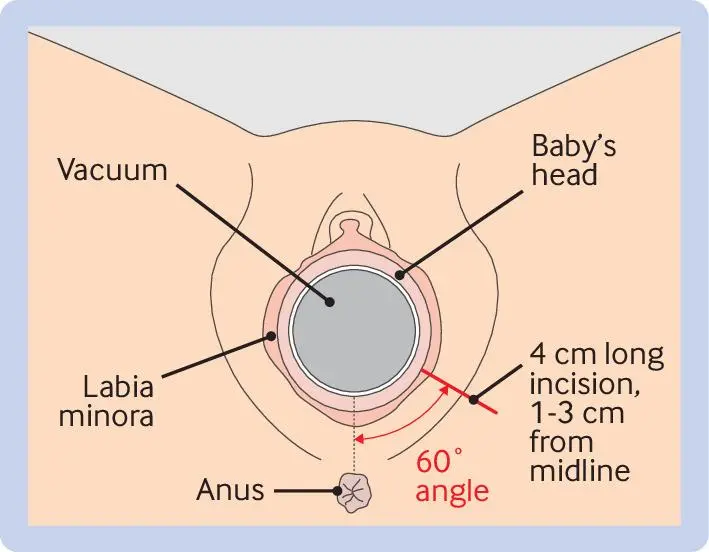
“Women giving birth for the first time and requiring instrumental birth are at the highest risk of sustaining OASI,” says , associate professor in obstetrics and gynaecology at the , Karolinska Institutet and senior consultant at the Department of Women’s Health, Danderyd Hospital. “Therefore, we wanted to assess if such injury could be prevented in this group with a lateral episiotomy (angled cut in the perineum) when the baby’s head is crowning.”
Participants were recruited to the EVA (Episiotomy in Vacuum Assisted delivery) trial at eight Swedish hospitals between 2017 and 2023. Over 6 100 pregnant women expecting their first child agreed to take part if the delivery required vacuum assistance. A total of 702 women with a vacuum assisted delivery were randomly assigned to receive a lateral episiotomy or no episiotomy.
The lateral episiotomy reduced the risk of OASI by an average of 53 per cent. Among the women assigned to the procedure, 6.1 per cent sustained an OASI, compared to 13.1 per cent in the comparison group. Moreover, the procedure did not increase the risk of severe blood loss, negative birth experience, prolonged hospitalisation or additional complications. However, the risk of wound complications such as wound infection and wound dehiscence was increased in the episiotomy group.
“Episiotomy as a medical intervention is controversial as it has historically also been used for normal births, sometimes without the woman’s consent,” says Sophia Brismar Wendel. “The use of episiotomy is highly variable in different countries, and in Sweden we’ve practised restrictive use given the lack of evidence. However, these results may impact obstetric care both in Sweden and elsewhere.”
The trial is also gathering data on the women’s self-reported symptoms at one and five years after childbirth. The results from the one-year follow-up will soon be analysed, which might give some answers about any differences in symptoms, such as anal incontinence and sexual function.
“This may help doctors and pregnant women in shared informed decision-making regarding the use of a prophylactic lateral episiotomy,” says Sophia Brismar Wendel.
The hospitals participating in the EVA study are the University Hospital of Umeå, Falun Hospital, Uppsala University Hospital, Danderyd Hospital, Stockholm South General (Söder) Hospital, Växjö Central Hospital, Sahlgrenska University Hospital – Östra, and Helsingborg Hospital. The study was primarily financed by the Swedish Research Council, Region Stockholm and the Uppsala-Örebro Regional Research Council. There are no reported conflicts of interest.
Publication
, Sandra Bergendahl, Maria Jonsson, Susanne Hesselman, Victoria Ankarcrona, Åsa Leijonhufvud, Anna-Carin Wihlbäck, Tove Wallström, Emmie Rydström, Hanna Friberg, Helena Kopp Kallner, Sophia Brismar Wendel, The BMJ, online 17 June 2024, doi: 10.1136/bmj-2023-079014.
Editorial about the study:








