During an initial mental health consultation, some people can exhibit overlapping symptoms consistent with multiple conditions – like (ADHD), , , and/or .
These challenges can be in addition to intra-illness heterogeneity – this is where individuals with an identical diagnosis, like schizophrenia, can show vastly different symptoms or combinations of symptoms.
Complex and overlapping symptoms can lead to adjustments in diagnosis over time, significantly delay treatment, increase disability and parental or family stress, as well as add to the broader .
Currently, there is a vast ‘translation gap’ between mental ill-health research and clinical integration of these research findings.
Although researchers have made unprecedented progress in identifying ‘averaged’ or ‘population-level’ mechanisms of mental health disorders, these approaches have led to a drowning effect at an individual level where person-specific information is often lost if it doesn’t align with an averaged expectation.
To bridge this gap between research and clinical practice, we have developed a novel individualised machine learning framework called .
By identifying personalised signatures that can be integrated into a clinician’s decision-making for each of their patients, Affinity Scores represent a fundamental shift in our approach to personalised psychiatry.
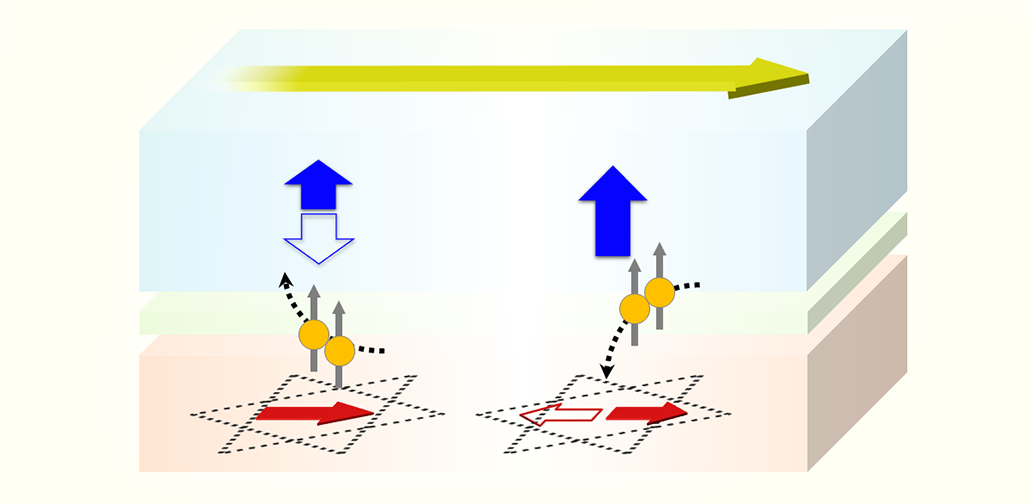
Simply put, Affinity Scores mimic clinical decision-making by comparing an individual to other people with a variety of clinical presentations.
They can combine an almost endless range of measures, including clinical markers for symptoms and quality of life, cognitive scores, brain structure and other higher-level or person-specific biomarkers.
Combining this data makes it possible to generate individual ‘fingerprints’, capturing differences between people with the same condition (intra-illness differences) and symptom similarities between people with different conditions (inter-illness overlap).
In this way, Affinity Scores not only predict diagnosis and prognosis but the unique, individual-level fingerprints can also be used by clinicians to determine factors that contribute most strongly to a person’s diagnosis.
Other benefits include the ability to identify , like anxiety or depression, determine patient strengths and areas of concern as well as help plan intervention strategies.
In our initial proof-of-concept study, recently published in , we examined the utility and diagnostic accuracy of Affinity Scores in a group of individuals with chronic and treatment-resistant schizophrenia, alongside healthy people.
In this study, we demonstrated that Affinity Scores had high predictive accuracy and, importantly, were able to differentiate individuals with treatment-resistant schizophrenia – the most severe form of this disorder – from those with chronic schizophrenia.
Affinity Scores also provided unique, individual-level fingerprints to highlight features contributing most strongly to a person’s score.
This allows clinicians to identify not only the most important treatment targets for any given individual, but also the areas of strength that might be leveraged to enhance treatment.
With the success of our proof-of-concept study, the next step is to translate Affinity Scores into a clinical decision-support tool.
An important part of this process will be to ensure that Affinity Scores not only work with rich research datasets, but also with the real-world data collected in a clinical setting.
To this end, we are collaborating with our clinical partners at to pilot our technology in a sample of children with ADHD, autism, as well as mood and anxiety disorders.
These pilot analyses have been incredibly promising, not only accurately identifying children’s pre-admission diagnoses, but also identifying comorbidities that were previously missed at admission but later picked up by the treating clinicians.
Most often this was because these other features were less obvious initially as they were dominated by the presenting symptoms.
Feedback from collaborating clinicians also indicated that the fingerprints provided by Affinity Scores identified factors potentially driving a child’s functional difficulties and may need focused intervention.
In effect, Affinity Scores identify patterns that are most often discerned by specialist clinicians with years of prior experience and make them available to clinicians with more limited expertise with these kind of disorders.
Dr Michelle Adams, a child and adolescent psychiatry registrar working in the Oasis inpatient unit, is a key collaborator on this project. She describes the utility of the Affinity Score framework in a clinical setting.
“There are few clinicians in Victoria with enough experience in neurodevelopmental disorders to have a mental database in which to fingerprint intuitively. It’s like we are borrowing their minds using Affinity Scores,” Dr Adams says.
Our hope is that this novel approach will result in a substantial shift in the current paradigm of diagnosis and treatment of mental health disorders, allowing clinicians to characterise their patients on a clinical, psychological, social and biological level to help better predict their diagnosis, potential comorbidities and illness prognosis.
These are critical first steps for improving the success of early intervention and prevention strategies and will be beneficial across all stages of illness.
For professional support, a good place to start is your family GP and/or mental health professional.
You can also call on 13 11 14 or on 1800 55 1800.
More resources for wellbeing include – a mental health service for young people and parents with apps and links to other sites; and – eating disorder support; – mental health information and support; – early intervention mental health services for 12-25-year-olds; – an online program for the prevention and treatment of childhood and adolescent anxiety; and – which provides crisis support and counselling.