In a global effort to improve the lives of breast cancer survivors, new leading health research has looked at strategies that can help prevent lymphoedema for millions of cancer survivors as a result of damage or removal of their lymph nodes during cancer treatment.
Compression sleeves, surgery to repair patients’ lymphatic systems and axillary reverse mapping (ARM) should be offered to people at risk of developing breast cancer-related arm lymphoedema (BCRAL), according to the study published by The Lancet in
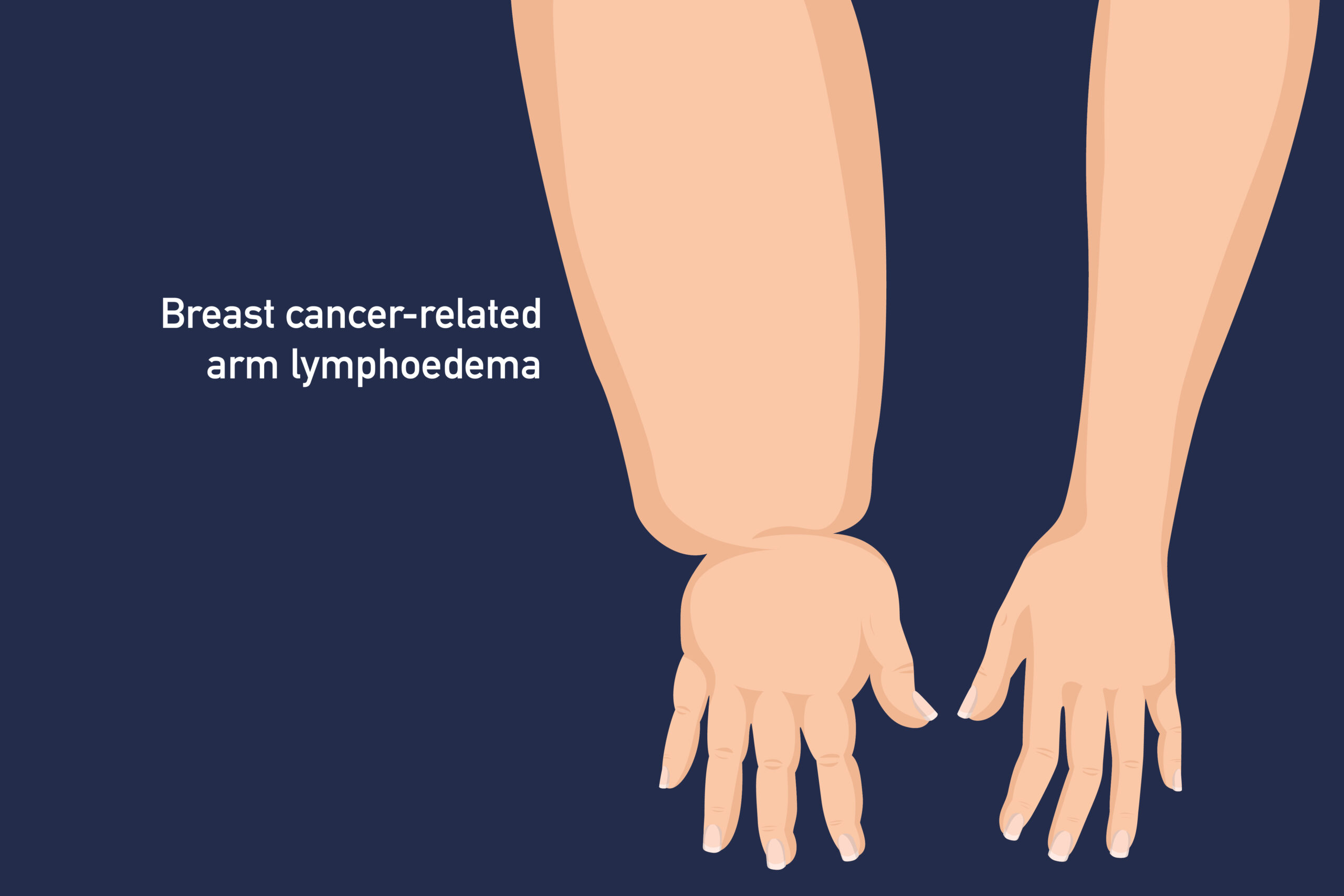
Lymphoedema is a distressing condition that involves the accumulation of fluid in patients’ arms, resulting from damage or removal of lymph nodes during breast cancer treatment. The global experts in this study have, for the first time, published a clinical guide on how and when to roll out evidence-based interventions.
While there is currently no approach that can completely prevent lymphoedema, researchers from Princess Margaret Hospital in Hong Kong, Flinders University and the University of Toronto collaborated with 64 global experts from 16 countries to develop guidance that can effectively help prevent the condition after reviewing clinical trials.
The study reviewed data from more than 60 thousand patients with breast cancer-related arm lymphoedema involved in high-quality randomised-controlled studies to determine the best prevention strategies and risk factors that can cause the condition.
These risk factors include post-surgery radiotherapy, not monitoring patients arm volume one month after surgery, the number of lymph nodes removed, and a high body mass index.
Breast cancer survivor Monique Bareham says chronic lymphoedema is irreversible, difficult to treat and significantly affects patients’ quality of life, so effective management to prevent it and halt its progression is critical.
“Like many breast cancer survivors, I received limited and conflicting information about lymphoedema following cancer treatment, leaving me anxious and ill-equipped to manage my symptoms. It had a negative effect on me psychologically and physically and left me unable to return to work. “
“This research raises awareness of this under recognised condition and addresses gaps in clinical understanding. It is a necessary step toward providing care that will lead to better health outcomes for many breast cancer survivors Worldwide.”

Deputy Vice-Chancellor (Research) at Flinders University and the study’s co-senior author, Professor Raymond Chan says about half of patients with breast cancer-related arm lymphoedema (BCRAL) develop this condition 12-30 months after surgery, but it can also develop many years later.
“Our study has revealed evidence-based approaches to prevent BCRAL through approaches that take into account risk factors for patients, the availability of treatment options and the expertise of healthcare providers to ensure all patients are offered effective interventions, regardless of where they’re receiving care.”
“This is the first study in the world to provide recommendations on the frequency and duration of surveillance, methods to detect early lymphoedema, thresholds for early intervention and types of treatments to offer depending on the degree of the condition. With this knowledge, these interventions can now be applied with confidence in clinical settings.”
Endorsed by the Multinational Association of Supportive Care in Cancer, experts support the rollout of surveillance programs that can help prevent lymphoedema and have for the first time backed treatments using compression sleeves.
Compression sleeves are designed to provide controlled pressure that reduces the swelling on the arms associated with patients going through treatment with breast cancer-related arm lymphoedema.
The lead author of the study, Dr Henry Wong, a clinical oncologist from the Oncology Department at the Princess Margaret Hospital in Hong Kong says this study is the first to provide a detailed guide on how to implement surveillance programs and prophylactic compression sleeves for the prevention of BCRAL.
“Our consensus-based recommendations generated by an international team of experts provide a strong voice for healthcare teams worldwide to adopt a proactive approach in preventing this irreversible treatment-related complication.”

Dr Matthew Wallen, a Senior Research Fellow within the Caring Futures Institute, and co-first author, says the strength of this clinical practice guidance document is in its robust multi-disciplinary approach to preventing BCRAL.
“By identifying key risk factors, implementing early surveillance, and providing recommendations around the latest treatment and management strategies, we can ensure people living with BCRAL are offered practical, timely, and evidence-based care interventions.”
“Our study sheds light on the best practices in the management of BCRAL and offers hope and empowerment to breast cancer survivors who may be devastated by their lymphedema,” says Dr Adrian Wai Chan, a clinical research fellow in the Department of Radiation Oncology, Sunnybrook Health Sciences Centre, the University of Toronto and co-first author.
The Lancet publication ‘Multinational Association of Supportive Care in Cancer (MASCC) clinical practice guidance for the prevention of breast cancer-related arm lymphoedema (BCRAL): international Delphi consensus-based recommendations’ is








