The tissue area that surrounds our teeth is known as the gingiva, and healthy teeth will nestle firmly into the gums thanks to the many gingival fibers that connect the tooth to the gingiva. The gingiva is home to fibroblasts – cells that contribute to the formation of connective tissue. A group of scientists from Tohoku University have discovered that the gingiva stiffness influences the properties of gingival fibroblasts, which in turn affects whether inflammation is likely to occur and make gingival fibers difficult to form.
Their findings were published in the journal Scientific Reports on January 24, 2023.
“We discovered that soft gingiva results in inflammation and hinders the development of gingival fibers,” says Associate Professor Masahiro Yamada from Tohoku University’s Graduate School of Dentistry.
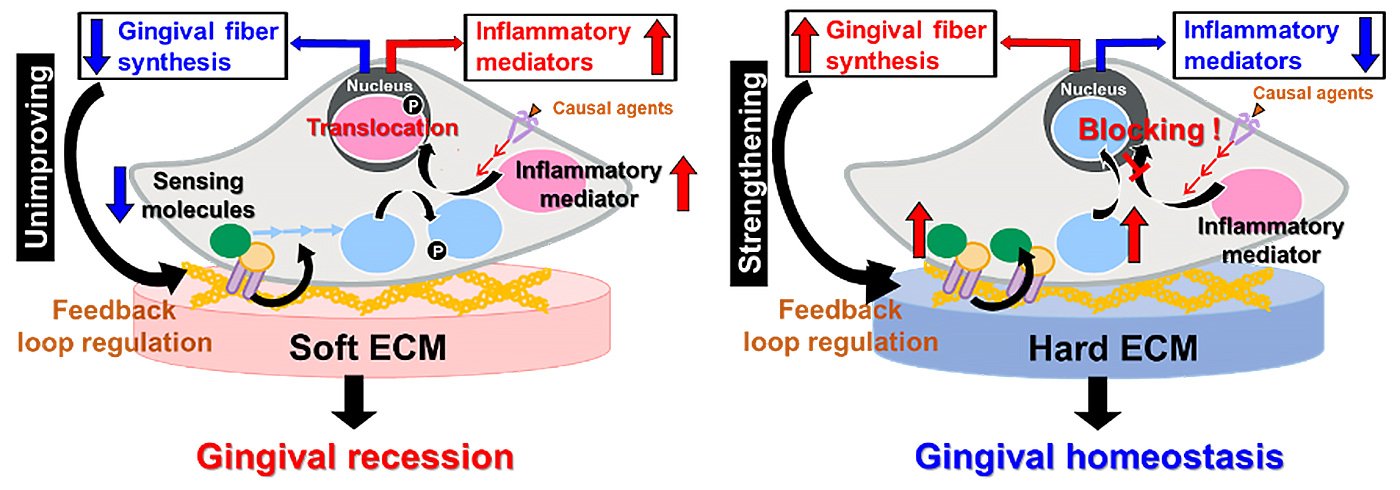
It has long been known that individuals with thick or stiff gingiva are less susceptible to gingival recessions. This is where the gingiva begins to recede and expose a tooth’s root. Many factors can lead to gingival recession, such as gum disease, over-brushing, and chewing tobacco. But this is the first time that gingival stiffness has been attributed to biological reactions.
Although fibroblasts play an important role in the maintenance, repair and healing of the gingiva, they also produce various inflammatory and tissue-degrading biomolecules which degrade the gingival fibers. In addition, fibroblasts are associated with immune responses to pathogens.
Yamada, along with his colleague Professor Hiroshi Egusa, also from the Tohoku University’s Graduate School of Dentistry, created an artificial culture environment that simulated soft or hard gingiva and cultured human gingival fibroblasts on them. They discovered that hard gingiva-simulated stiffness activated an intracellular anti-inflammatory system in the gingival fibroblasts that prevented inflammation. Yet, soft gingiva-simulated stiffness suppressed the fibroblastic anti-inflammatory system. This increased the likelihood of inflammation and resulted in less collagen synthesis.
“Our research is the first to demonstrate the biological mechanisms at play in regards to a patient’s gingival properties,” adds Yamada. “The results are expected to accelerate the development of advanced biomaterials to control local inflammation or microdevices that simulate the microenvironment of inflammatory conditions.”
- Publication Details:
Title: Substrate stiffness controls proinflammatory responses in human gingival fibroblasts
Authors: Watcharaphol Tiskratok, Masahiro Yamada, Jun Watanabe, Nadia Kartikasari, Tsuyoshi Kimura, Hiroshi Egusa
Journal: Scientific Reports
DOI:







