Researchers from Karolinska Institutet have in collaboration with the University of Eastern Finland and Lund University a new publication in Genome Biology, demonstrated that targeting cell cycle and cell fate regulatory programs blocks non-genetic cancer evolution in acute lymphoblastic leukemia.
Findings from in collaboration with the group of the University of Eastern Finland and , Lund University shed light on the intricate connections between gene regulation, cell cycle control, and cell fate, providing a rationale for combining WEE1 inhibitors with other targeted therapies to enhance treatment efficacy while minimizing side effects.
B-cell acute lymphoblastic leukemia (B-ALL), the most common childhood cancer, accounts for about 30% of all childhood cancers and presents significant treatment challenges. Regardless of the effectiveness of standard chemotherapeutic protocols and advances such as allogeneic hematopoietic stem cell transplantation, approximately 15-20% of patients continue to experience poor outcomes due to non-responsiveness or relapse after therapy. Importantly, intensive and extended treatment protocols result in almost 80% of childhood ALL survivors experiencing life-threatening medical complications by the age of 45.

Despite the promise of precision treatments, the diverse characteristics of cancer cells present limitations. In a recent study that focused on targeting the WEE1 kinase, a pivotal protein in cell cycle checkpoints, promising results emerged. Through detailed analysis of KMT2A-rearrangements leukemia cells, the research team discovered that while a significant portion of cells experienced cell death from WEE1 inhibition, a subset instead transitioned into a drug-tolerant state. “Surprisingly, these drug-tolerant cells displayed activation of differentiation and survival programs related to pre-B cell receptor signalin” says , PhD at the shared these findings.
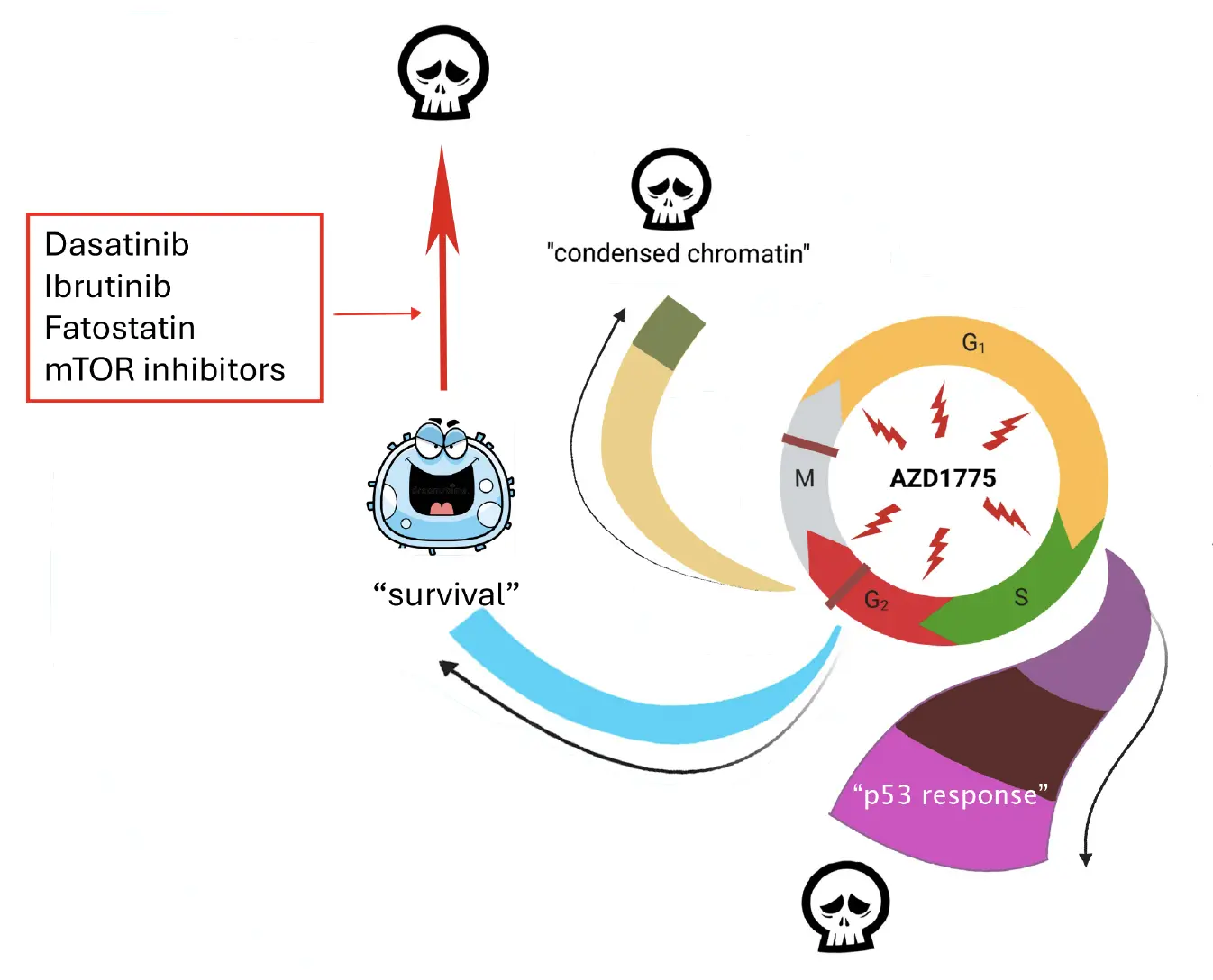
Illustration: Aljona Maljukova
Contrary to the traditional view that primarily links stemness features to drug resistance in ALL, our findings reveal a different perspective and proposes that targeting vulnerabilities in cell cycle regulation can lead to drug-tolerant cells displaying a more differentiated phenotype and reduced stemness traits. Analysis of drug responses in MEF2D rearranged leukemia cells obtained from patients supports this notion and shows that leukemic cells that survive chemotherapy shifts towards a pre-B cell-like state, differing from their less differentiated pro-B phenotype observed at diagnosis. These results suggest a common resistance mechanism among various ALL subtypes, as leukemic cells adapt to treatments by activating similar transcription factor pathways. Understanding these mechanisms holds the potential to pave the way for more effective therapeutic approaches, ultimately enhancing patient outcomes.
Building upon these findings, the team identified several drugs targeting pro-survival pre-B cell receptor signaling, that when combined with WEE1 inhibitors in a sequential treatment strategy, effectively counteracted drug tolerance, prevented recovery post-treatment and induced cell death in xenograft KMT2A-r models.
“Moving forward, we aim to investigate whether the changes in transcription factor activities are part of a broader stress response in leukemia¨. Specifically, we will explore whether chemotherapy agents used in standard leukemia protocols also contribute to the activation of a differentiated pre-B-like program, potentially leading to drug tolerance. We hope that this research will contribute to our understanding how drug treatments relate to cancer cell diversity and therapy resistance. The goal is to define effective combination therapies capable of countering heterogeneity and preventing disease recurrence.” says Principal Researcher at the Department of Cell and Molecular Biology.
Important collaboration partners
- The Institute of Biomedicine, School of Medicine, University of Eastern Finland,
- Division of Clinical Genetics, Department of Laboratory Medicine, Lund University,
- Tampere University Hospital
Main financiers of the study
The Swedish Childhood Cancer Fund, Swedish Cancer Society, The Swedish Research Council, the cancer Research Funds of Radiumhemmet, AstraZeneca, Academy of Finland, H2020 European Research Council,
Publication
Alena Malyukova1*†, Mari Lahnalampi2†, Ton Falqués‑Costa3, Petri Pölönen2, Mikko Sipola2, Juha Mehtonen2, Susanna Teppo4, Karen Akopyan1, Johanna Viiliainen1, Olli Lohi4, Anna K. Hagström‑Andersson3, Merja Heinäniemi2*† and Olle Sangfelt.
Genome Biology (2024) 25:143








