When it comes to finding a long-lasting treatment for depression, a team of Toronto researchers says it could come down to finding the perfect rhythm.
The approach, under development by scientists at Sinai Health, the Centre for Addiction and Mental Health (CAMH) and the University of Toronto, has nothing to do with music and everything to do with tweaking an existing form of brain stimulation therapy.
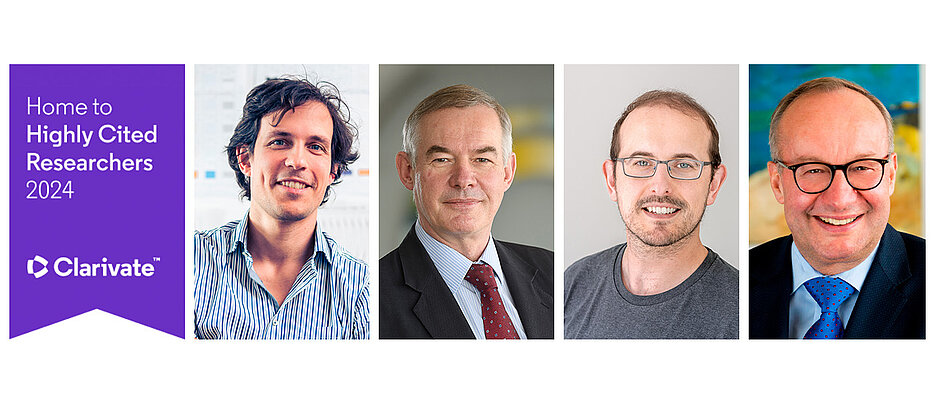
To improve the technology and test it in patients, four researchers have today been awarded a grant by .

Tarek Rajii
“It is a very exciting collaboration that combines bench and bedside research in the same project,” said Tarek Rajji, principal investigator and clinical lead on the project.
Rajji is executive director of the Toronto Dementia Research Alliance (TDRA) and chief of the adult neurodevelopment and geriatric psychiatry division at the Centre for Addiction and Mental Health (CAMH), as well as a Clinician Scientist in CAMH’s Campbell Family Mental Health Research Institute. He is also an associate professor in the Temerty Faculty of Medicine’s department of psychiatry.
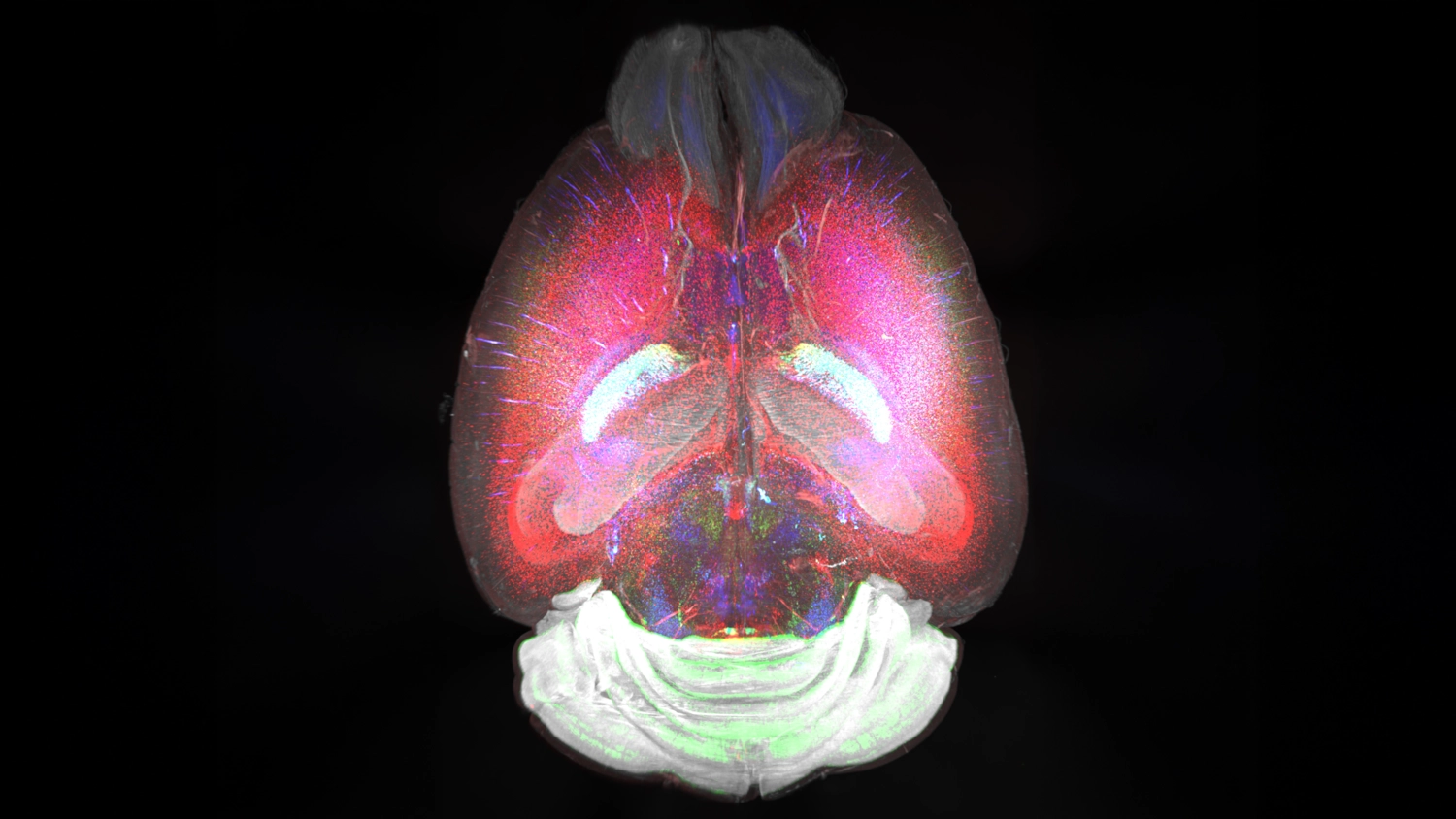
The research centres around transcranial magnetic stimulation, or TMS, a form of brain stimulation therapy that’s been shown to hold enormous promise in helping patients with treatment-resistant depression. The approach uses a device to deliver pulses of magnetic stimulation to the prefrontal cortex, a part of the brain associated with mood regulation.
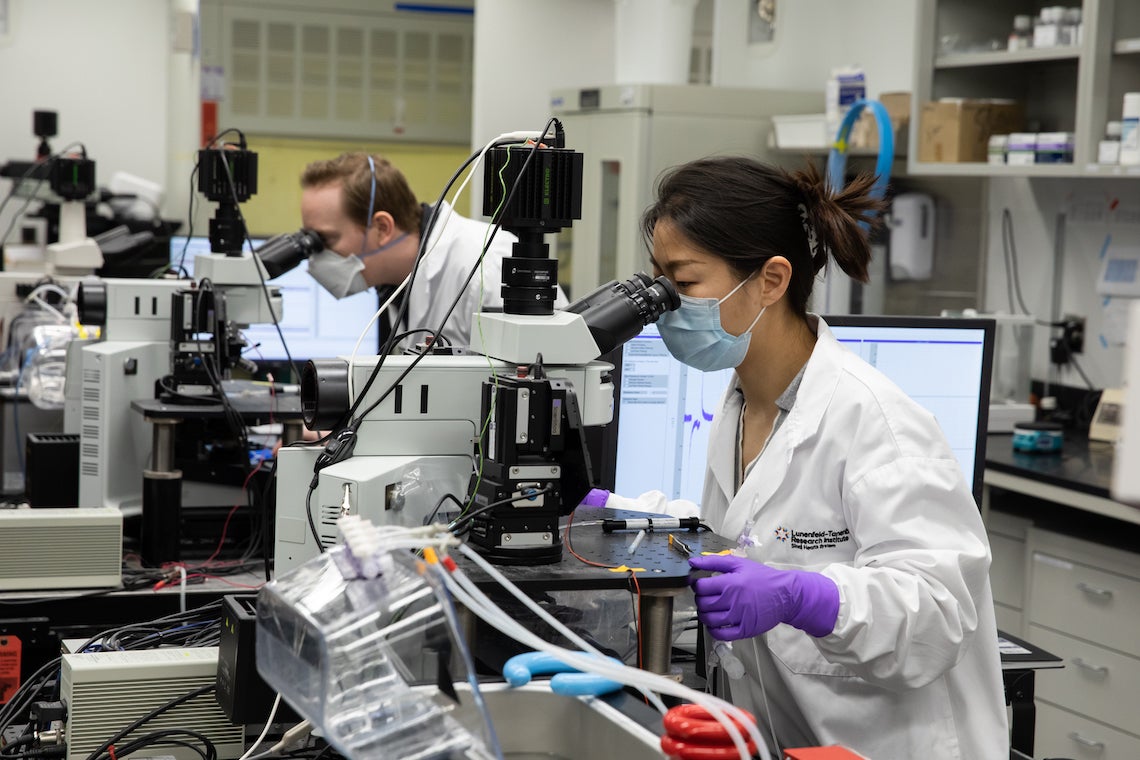
The basic science component of the project involves brain stimulation to determine whether changing the spacing or tempo of the pulses to the brain could ultimately deliver long-lasting relief from depression symptoms.

Graham Collingridge
“The pattern of stimulation is vital,” said Graham Collingridge, a senior investigator at Lunenfeld-Tanenbaum Research Institute (LTRI) at Sinai Health and a professor of physiology and director of the Tanz Centre for Research in Neurodegenerative Diseases at Temerty Medicine. “It has been recently discovered that instead of applying the rhythm within a short space of time, [if] you have a break for a few minutes and then repeat the stimulation, the effect on synapses in the brain is stronger and longer-lasting.”
Collingridge studies a process called long-term potentiation, in which a brief period of intense neuronal activity leads to a long-lasting increase in the strength of connections between the nerve cells.
To find the perfect pattern, Rajji and Collingridge are collaborating with Evelyn Lambe, an associate professor of physiology at Temerty Medicine, who is leading the work to optimize the stimulus parameters in the prefrontal cortex, the region targeted by TMS in patients, as part of the Bell Let’s Talk Brain Canada research grant.

Evelyn Lambe
“The goal is to optimize treatment to rebuild connections between neurons essential for mood regulation,” said Lambe.
Her lab’s work investigating the impact of social isolation on the brain has become increasingly relevant to mental health during the COVID19 pandemic. “Social isolation and other stressors wear us down by impairing brain function at the cellular level,” Lambe notes.
Rajji, meanwhile, will adapt the optimized stimulation parameters to humans using TMS and electroencephalograhy. His team will examine which pattern of stimulation leads to better brain plasticity in the frontal lobes of adults with acute depression.

Sanjeev Sockalingam
Throughout the project, Sanjeev Sockalingam, a clinician-scientist and vice-president of education at CAMH, and professor of psychiatry at Temerty Medicine, will lead the knowledge translation component of the work. This will involve mental health clinicians, people with lived/living experience and families working with researchers from the start of the project.
“The integrated approach involving clinicians and service users will help us co-create knowledge that gets to people who can use it faster and more effectively,” said Sockalingam.
With files from Sinai Health, the Centre for Addiction and Mental Health and U of T’s department of physiology.