Almost six people a day die from drug overdoses in Australia.
In its 2018 overdose report the Penington Institute revealed that more than 1,700 drug related deaths in Australia were accidental, and most of these involved prescription medications.
Now Victoria has started to roll out a ground-breaking cloud-based real-time prescription monitoring system to medical practitioners and pharmacists that will perform a key role in helping to reduce the risk for many of these avoidable deaths. To set this in context, in 2017, 414 Victorians died from this problem, more than the State’s road toll.
Called SafeScript, the new system monitors the prescription and dispensing of all controlled (Schedule 8) medicines such as morphine and oxycodone, as well as other higher risk medicines including codeine and diazepam. Coupled with an education initiative for consumers and practitioners, the Victorian Department Health and Human Services (DHHS), is confident that its $30 million investment will rein in accidental deaths by overdose across the State and set a benchmark for other States and Territories that do not currently have such a system.
As Matthew McCrone, director of real time prescription monitoring implementation for DHHS, explains; “The problem is that too many people are dying from prescription medicines, from overdose. That number is ever-growing. We have had things in place for a very long time in Victoria, to regulate these high-risk medicines; clearly, we needed to transform how we go about doing this, in order to prevent these deaths occurring. So, preventing deaths from prescription drug overdose is why we’re doing this. And the way to get there is to help doctors and pharmacists make more informed clinical decisions and thus facilitate safer prescribing and dispensing of these high-risk medicines.”
SafeScript connects to pharmacy and GP software to streamline workflow. “It is, ultimately, about making sure that the clinician has information in front of him or her, at the point that they’re needing to make a decision about whether to prescribe a particular medicine or dispense it. So, SafeScript provides them that information in as seamless a way as possible. Equally important – and, this is the other thing that we need to deliver – is that the clinician knows what to do next.
“If they have information in front of them that they wouldn’t have otherwise had – for example, that that patient is seeing other doctors or is on other medicines, which means the medicine they were considering is even more risky – the clinician needs to know what they’re going to do next. How are they going to support that patient so that things work out safely for them? That’s why the workforce training that we’re delivering is part of the project. It’s so utterly crucial to the overall objectives of the project.”
https://www.penington.org.au/australias-annual-overdose-report-2018/
“The problem is that too many people are dying from prescription medicines, from overdose. That number is ever-growing. We have had things in place for a very long time in Victoria, to regulate these high-risk medicines; clearly, we needed to transform how we go about doing this, in order to prevent these deaths occurring. So, preventing deaths from prescription drug overdose is why we’re doing this. And the way to get there is to help doctors and pharmacists make more informed clinical decisions and thus facilitate safer prescribing and dispensing of these high-risk medicines”. – Matthew McCrone, director of real time prescription monitoring implementation for DHHS
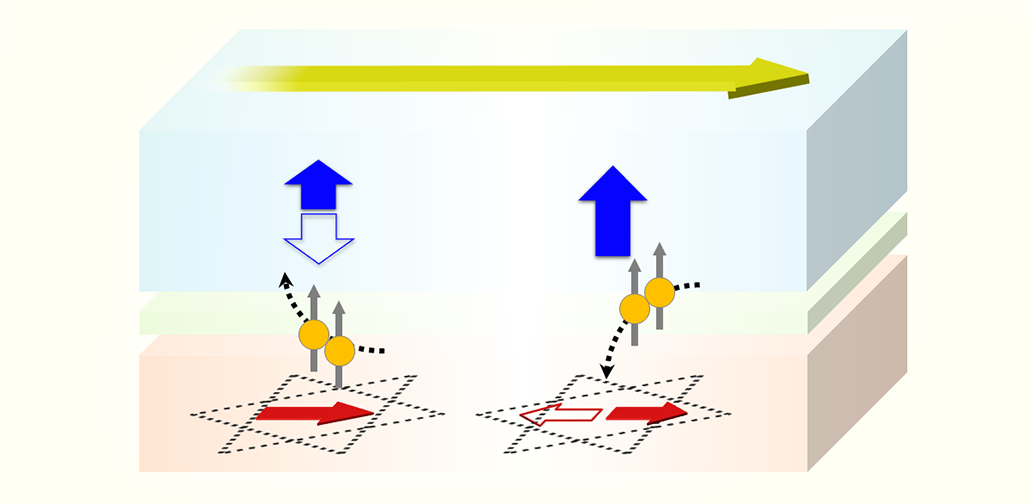
Real time alerts
Developed by specialist pharmacy solution provider Fred IT Group, SafeScript offers doctors and pharmacists a real time alerting capability. If the system detects that a patient has gone to multiple providers for the same medicine over a short period of time, or they are using a risky combination of medicines that elevates the risk of overdose, it will automatically raise an alert.
A staged roll out is underway, with the first implementation live across the Western Victoria Primary Health Network since the start of October 2018, ahead of a statewide roll out in April 2019. From April 2020, every medical practitioner and pharmacist in Victoria will need to access SafeScript before they dispense or prescribe the monitored medicines.
Being based on Microsoft’s trusted Azure cloud ensures the security needed by such a sensitive application, but also provides the scalability and reach which will be required as the solution is rolled out across Victoria, and the flexibility to monitor new medications as required. System performance and resilience is also critical; one of DHHS’ technical requirements was that the system needed capacity to support the potential use by all Victoria doctors and pharmacists (more than 30,000 clinicians) at any time.
Paul Naismith, CEO of Fred IT Group (Fred), who is also a pharmacist, says that the system has been designed so that the information is presented to the clinician or pharmacist in less than three seconds. “We couldn’t have done this without the maturity of Azure.”