In the realm of medical anomalies, few conditions captivate curiosity and concern quite like , commonly known as “water allergy”.
Authors
Samuel J. White
Senior Lecturer in Genetic Immunology, Nottingham Trent University
Philippe B. Wilson
Professor of One Health, Nottingham Trent University
This rare affliction transforms the seemingly innocuous act of water contact into a tormenting ordeal, afflicting people such as 22-year-old from South Carolina, US.
Diagnosed with water allergy, Montefusco’s life is marked by the excruciating sensation of a burning itch deep beneath her skin. This is triggered by the mere touch of water. Her account reveals the harrowing experiences faced by those grappling with this puzzling condition.
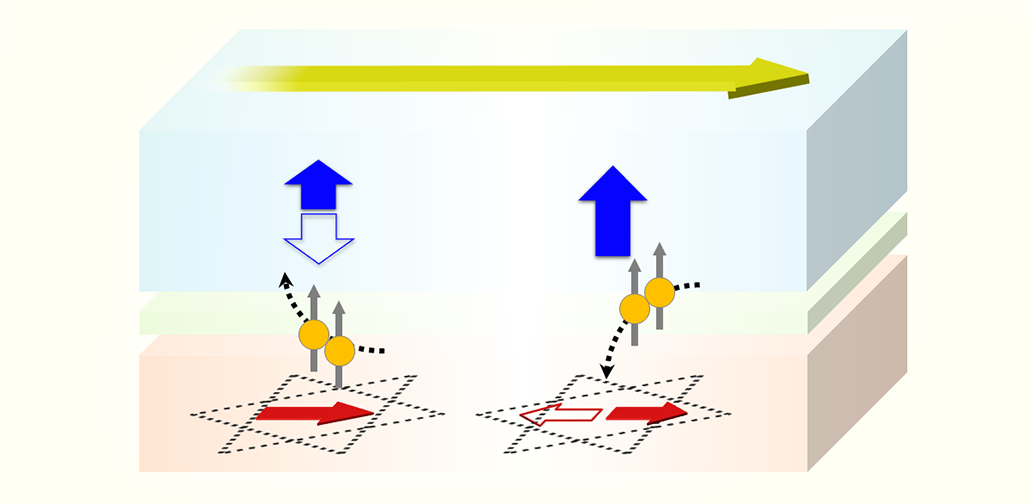
At its core, water allergy is believed to arise from an triggered by water’s interaction with the skin. Think of your immune system as a vigilant guardian, always on alert for invaders. In aquagenic urticaria, water somehow . This leads to the release of substances like histamine – causing hives, welts and itching.
Researchers have pinpointed mutations in associated with water allergy, such as the FABP5 gene, crucial for skin barrier function. Mutations in this gene disrupt the skin’s ability to repel water, activating an inflammatory response.
Variations in in immune regulation and skin integrity also contribute to susceptibility. However, environmental factors such as hormonal changes or chemical exposure can influence its severity.
Understanding the genetic basis offers insights into how the disease occurs and potential therapies. By identifying specific genetic markers, personalised treatment approaches targeting underlying mechanisms can be developed.
Despite these strides, much about water allergy remains unknown. However, by integrating insights from genetics, immunology and dermatology, scientists aim to unravel the secrets of this rare water allergy, offering hope for improved diagnosis and management.
The first documented mention of water allergy dates to the , with case reports detailing the perplexing experiences of people afflicted by water-induced hives.
Since then, sporadic cases have dotted medical literature, contributing to our of this ailment. Recent trends suggest a gradual increase in cases, driven by heightened awareness among healthcare professionals and improved diagnostic capabilities.
Water allergy’s rarity adds to its mystique. Despite its obscurity, the condition leaves an indelible mark on those affected, shaping their experiences in profound and unexpected ways. Current estimates suggest that have been reported globally. This underscores its status as one of the rarest form of hives.
Managing this allergy presents a formidable challenge for patients and healthcare providers alike. Here are the strategies used.
Treatments
Conventional allergy treatments () offer temporary relief but may not address the underlying cause.
Experimental therapies such as (exposing the skin to ultraviolet light) aim to calm the immune response and reduce inflammation. This therapy has shown some promise in alleviating symptoms.
Biologic agents, so-called “large-molecule drugs” made from proteins, target specific immune pathways implicated in allergic reactions. They offer a more that holds potential for .
Avoiding water is tricky and involves careful planning, including .
Using , such as emollient creams, can help create a layer between the skin and water, which may help reduce symptom severity and frequency.
Psychological support
provide a safe space for people to navigate the emotional difficulties associated with living with a chronic and misunderstood condition like aquagenic urticaria.
Offering coping strategies and fostering resilience can empower patients to better cope with the uncertainties and stressors of their condition, improving overall quality of life.
into immune system mechanisms underlying aquagenic urticaria is essential to finding new treatments.
Continued clinical trials and studies are crucial to evaluate the efficacy and safety of emerging therapies, such as phototherapy and biologic agents, in managing aquagenic urticaria. Unfortunately, these studies are limited by .
![]()
The authors do not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and have disclosed no relevant affiliations beyond their academic appointment.